KERATOCONUS
What is Keratoconus?
Keratoconus is a progressive corneal disease. It occurs when the normally round (dome-shaped) cornea thins and gradually bulges outwards into a cone shape. It is relatively rare, affecting approximately 1 in 5000 people, although the numbers affected do vary in different ethnic groups.
What causes Keratoconus?
Keratoconus is commonly associated with excessive eye rubbing, chronic eye inflammation and some connective tissue disorders. Conditions which cause eye irritation and rubbing such as asthma, hay fever and eczema are commonly associated with keratoconus.
Hereditary factors are also important in the diagnosis of keratoconus. The disease is more prevalent in certain races such as Middle Eastern and Pacific Islanders.
New research that has come out also suggests that the weakening of corneal tissue that leads to this abnormal thinning can be due to imbalance of enzymes within the cornea.
What are the signs and symptoms?
The cone shaped cornea often causes progressive refractive changes and irregular astigmatism to develop. This often leads to symptoms of distorted and blurred vision. Typically night vision is affected first with starbursts, haloes and streaks of light. Later daytime blurring of vision is also noticed.
Patients with keratoconus often notice symptoms between the ages of 10 to 25. This progressive disease often affects both eyes, although the two eyes can be affected to different degrees.
Other commonly reported symptoms:
- Excessive eye irritation including severe itchiness/ excessive eye rubbing
- Headaches/ reported eye strain
- Increased glare and light sensitivity
- Reported difficulty with night driving / ghosting around lights
- Continual changes to glasses

How is Keratoconus Diagnosed?
Often patients are referred to an ophthalmologist from an optometrist. Optometrists often refer patients on when they notice continual changes to glasses prescriptions and increased astigmatism, in a short amount of time.
Tests to diagnose keratoconus:
- Vision check
This is a standard test done routinely to patients having a full ophthalmic exam. Often patients with keratoconus display poor vision often worse in one eye. - Refraction
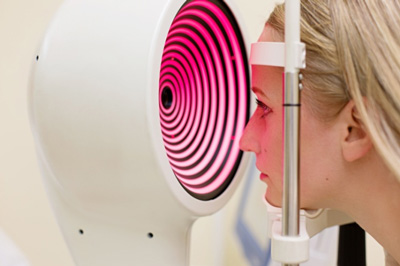
Ophthalmologist will check your optical prescription to see what best corrected vision is. The common refractive outcome in keratoconic patients is a high degree of astigmatism - Corneal Topography
Corneal topography is an optical scan that takes a map of the corneas surface and measures the thickness of the cornea. Patients who displaykeratoconus often display abnormally thin central corneas. In advanced keratoconus is can also show scarring to the cornea. Corneal Topography is the best and most accurate way to diagnose keratoconus. - Keratometry
This is technique where the ophthalmologist shines a light onto the cornea. The reflection determines the curve. This is a more rudimentary measurement compared to corneal topography.
Keratoconus Treatment:
Early Treatment (Mild-moderate keratoconus):
In the early stages of keratoconus often updated glasses or soft contact lenses are prescribed. The ophthalmologist will often recommend 6 monthly checkups or to present if there is a noticeable change to vision. Patients will be instructed to avoid eye rubbing and use allergy drops to reduce the incidence of this which can cause progressive thinning.
Progressive Keratoconus:
As the disease progresses and the cornea continues to thin it often becomes more irregular in shape and glasses and soft contact lenses can often not provide optimal vision.
Rigid Gas permeable contact lenses
These are hard contact lenses and are often the first step to treating progressive keratoconus.
Hard lenses cause a compression of the cornea to reduce the “bulging” caused by the disease .It offers a more uniform area of the cornea and often patients notice clearer vision.
Patients often complain of initial discomfort but the advantage is that they are custom made to fit the individual cornea. Frequent visits to the optometrist to change prescription and fittings are one of the major draw backs.

Corneal Rings including INTACS and Kerarings
These are best described as tiny plastic inserts which are crescent shaped. They are inserted just under the eyes surface into your cornea and promote flattening and continue to support the shape of the cornea which gives more functional vision.
Studies have proven that these rings can give an average of two lines of improvement on a standard vision chart.
Another advantage is that they are more tolerable than contact lenses and are removable and exchangeable. The surgical procedure normally takes a short amount of time of about 10 minutes.
Disadvantages are that like with any surgical procedure there is always the risk of complication, infection and injury to the eye during the procedure.
Collagen Cross Linking (UVX):
Collagen cross- linking is a procedure where the corneal tissue is strengthened through the use of vitamin drops (riboflavin) and UV light. Cross linking is very effective at stopping the progression of keratoconus. It is therefore most beneficial at the earlier stages of keratoconus to help preserve good vision. In some cases, cross linking can improve vision however the main reason for performing cross linking is to prevent further progression.
The most effective way to perform cross linking is the “epithelium off” method. This means that the outer portion of the cornea (epithelium) is removed to allow better absorption of the riboflavin vitamin B drops into the cornea which is then activated by the UV light.
The procedure takes around 1 hour. The first 30 minutes involves drops every two minutes and then the accelerated 9 minute UV light is applied. During the procedure anaesthetic drops are applied to keep patients comfortable. After the procedure patients are given instructions to use drops for a month after the procedure and to wear a hard eye shield to bed.
Post operatively the first two days the eye can be quite painful for the patient as the epithelium heals over the first 48 hours. Promotion of comfort and healing is done through the insertion of a bandage contact lens after the procedure.
Patients will not notice any great improvement to vision initially as it takes up to 6 months for the cornea to settle down. The main outcome will be to stop progression of the disease and in some cases patients notice a line of vision improvement.
At South West Institute we are very happy to be one of the few practices in the south west to offer this treatment locally in our practice. Dr Tess Huynh and Dr John Males have over 6 years experience being one of the first surgeons in Australia to offer this advanced technique in keratoconic treatment.
Topography guided laser+ collagen cross-linking:
This is one of the newest techniques available for the treatment of progressive keratoconus.
Laser treatment has previously not been available for patients with keratoconus.
Topography guided laser is able to restore the cornea from its bulging state to a more regular corneal surface and then collagen cross linking is applied to promote this new shape and stabilise in this new shape. It does not eliminate the need for glasses or contact lenses but in most circumstances reduce the strength of glasses and aids in better contact lens fittings, giving patients clearer vision.
In some circumstances corneal transplantation may still be necessary in more advanced cases of keratoconus.
Dr John Males and Dr Tess Huynh are at the forefront of treatment and are one of the few specialists in Sydney to offer this.
Cornea Transplant:
In patients that have progressive keratoconus where there is extreme corneal thinning/scarring it is likely corneal transplant will be necessary.
This means that the patient’s tissue is replaced with healthy donor tissue. Patients may still need to wear optical correction such as glasses and contact lenses and may need further laser treatment in the future.
In Australia corneal transplant is generally a successful procedure but there can be complications such as graft rejection, astigmatism which increases difficulty to wear contact lenses, infection and poor vision.