Age Related Macular Degeneration
What is the Macula?
The macula is a light sensitive pigmented tissue located centrally within the back of the eye known as the retina. The macula is our central vision and we use it to read fine print, form as well as see colour and recognise faces.
What is Age Related Macular Degeneration (AMD or ARMD)?
ARMD is one of the leading causes of blindness in the over 50 year old Australian’s. It is most commonly found in the Caucasian population.
ARMD causes the light sensitive tissue and cells within the retina to break down. This can cause blurred vision, distortion and central visual loss.
This condition is a chronic problem which there is no known cure. Patients should be monitored or managed regularly by their Ophthalmologist. Advancement of this disease will not cause total blindness however there will be central visual loss.
What are the risk factors for Macular Degeneration?
The direct cause of ARMD has not been identified however both heredity and environmental factors such as smoking may contribute to this disease.
What are the symptoms of Macular Degeneration?
Macular degeneration early symptoms include:
- Straight lines appear distorted.
- Missing, or jumping letter/words when reading
- Dark, blurry, grey spots appear in the central vision.
- There are several eye conditions that have similar symptoms therefore it is prudent to see your Ophthalmologist to diagnose the condition.
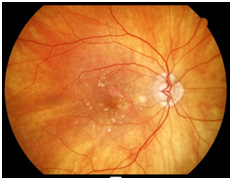
Types of ARMD
Dry Macular Degeneration – The dry form can produce gradual loss of vision. There is atrophy (Wasting away) of the retinal
tissue and yellowish metabolic wastes deposited (Drusen) in the retina.
Wet Macular Degeneration –The wet form commonly known as the active ARMD. Abnormal vessels from underneath the retina break through causing bleeding and scarring into the retinal layers.
How is Age Related Macular Degeneration diagnosed?
Tests below will help diagnose ARMD;
Vision testing: Assessing central vision.
Amsler Grid: A card with a grid to assess distortion or blurred spots.
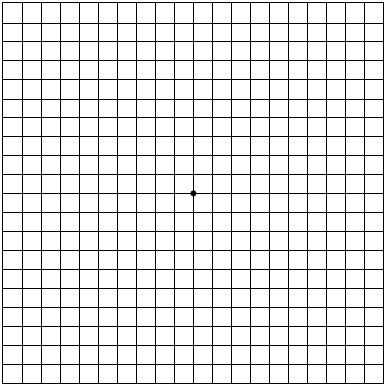
How to Test Yourself with the Amsler Grid
Patients who wear reading glasses should wear them when looking at the Amsler grid. Hold the grid at approximately reading distance which is about 30cms away.
To do the test properly cover one eye and focus on the central spot.
Things to look for:
- Do any of the lines appear distorted, wavy or blurred? ( A normal examination all lines will be straight )
- Do any areas on the grid appear dark or missing?
- Are you able to see all corners and sides of the grid?
- Don’t forget to test both eyes.
VERY IMPORTANT: Report any irregularity to your eye doctor immediately.
FFA (Fundus Fluorescein Angiography): 5ml of Fluorescein dye is injected into the arm and photographs are taken of the retina to assess for active ARMD. This test takes about 15 minutes to do.
OCT Scans (Optical Coherence Topography: It is a non-invasive scan of the macula to identify retinal structural changes and fluid.
Comprehensive eye examination: After dilatation of the pupils, the Ophthalmologist can diagnose for ARMD.
Treatment/Management
The progression of Dry ARMD can only be slow down through diet and lifestyle changes. Usually it is recommended to:
- Take vitamins based on the AREDS formula.
- Eat healthy nuts.
- Eat low Glycaemic index (GI) carbohydrates
- Eat green leafy vegetables and fresh fruit daily.
- Eat fish meal 2-3 times a week.
- Quit smoking.
Wet ARMD also can only be slowed down through diet and lifestyle changes. This active condition can be arrested with a course of the follow treatments below:
Laser
Laser is rarely used to treat wet ARMD. It will cause permanent scarring and a blind spot. It can be used where fluid and bleeding is away from the macula.
Visudyne Photodynamic therapy (PDT)
Approximately 30ml of Visudyne dye is gradually injected into the arm over a ten minute period. Patient may experience back pain during the injection period.
This is followed by a cold laser by the Ophthalmologist to block the leakage in the retina (The laser does not scar the retina).
Patient must cover up their whole body from sunlight for 48 hours after treatment.
Visudyne was initially used to treat wet ARMD over ten years ago. However intravitreal injections (Injection into the white part of the eye ball) are now the primary form of treatment.
Visudyne is sometimes used as co therapy treatment with intravitreal injections in some cases.
Intravitreal Injections
Currently intravitreal injections are the primary form of treatment for this condition. Drugs such as Avastin, Lucentis and Eylea are used to inject into the white part of the eye known as the sclera.
These are anti –VEGF (Vascular Endothelial Growth Factor) drugs. VEGF are proteins within the eye that trigger the growth of abnormal vessels and fluid accumulation within the retinal layers.
Avastin, Lucentis and Eylea are used to treat this. Initially 3 courses of injections are given, normally 4 weeks apart. Usually a patient can expect about 7 injections within the first 12 months.
The primary aims of these drugs are to dry out the fluid in the retina and hold the vision to its current level. Patients have reported some visual improvement.
Avastin (Bevacizumab): Is non TGA (Therapeutic Good Administration) approved drug that has been used by Ophthalmologist around the world for over 10 years. It has been proven to be quite effective.
Lucentis (Ranibizumab): Is a TGA approved drug. It has been used for the past ten years and is one the most highly effective drug available.
Eylea (Aflibercept): Is a TGA approved drug. It has been used for the past two to three years and is one the most highly effective drug available.
What are the risks/side effects of Intravitreal injection?
A patient may experience some irritation, grittiness and sandy sensation following the injection. The eye may water and usually settles down the next day. The antiseptic used to prepare the eye for the procedure may cause this sensation.
The Ophthalmologist may prescribe their patients antibiotic eye drops or ointment after the injection.
As with any minor surgery procedure there is a small risk of complication such as infection of the eye. Usually this can be treated with medicated drops and injections, but in some cases permanent vision loss can result.