Paediatrics
At South West Vision Institute we pride ourselves on thorough eye examinations for children. Please note that at your initial consult your child may have up to 3 examinations. Your child’s eyes will also need to be dilated, where the pupils are opened with eye drops so the doctor can see into the back of the eye. In children with dark eyes the dilating process may take over an hour. Please allow at least 3 hours for your child’s first visit.
Amblyopia (Lazy Eye)
Amblyopia is where a child’s vision does not fully develop due to misalignment of the eyes or blurred vision. It is the most common cause of childhood vision problems.
Vision in children starts developing from birth. Initially a baby’s vision is very poor but as the child grows and light continues to stimulate the eyes the vision improves. Near vision develops first followed by distance vision. By around the age of 4 a child should be able to clearly focus for the distance. From this age the brain slowly consolidates the vision until around 8 years old. This means that after this age any amblyopia that has not been treated is extremely hard to improve. Therefore it is important that if you suspect your child has poor vision that they are seen and treated before this age.
Causes
- A need for glasses in one or both eyes
- Strabismus (misalignment of the eyes)
- Nystagmus (shaking eyes)
- Ptosis (droopy eye lid)
- Childhood cataracts
Symptoms
Amblyopia is typically very hard to detect in young children as they will not complain that their vision is blurry. The most effective method of detection is having your child’s vision assessed. However please make an appointment with us if you notice your child:
- Regularly shuts one eye
- Complains they can’t see when one of their eyes is covered
- Regularly rubs one eye
- Has a turned eye
- Has a white pupil
- Has eyes that shake

Treatment
To develop normal vision the child must use their amblyopic eye which often requires the child to wear a patch over their good eye. This usually needs to be performed for at least 2 hours per day. Alternative methods include prescribing eye drops, wearing vision filters or manipulating the strength of the glasses.
A wide assortment of eye patches is available at South West Vision Institute which you can purchase at any time from our reception. We stock both adhesive and fabric patches. Our fabric patches which attach to glasses come in several different sizes with a variety of colourful themed patterns for boys and girls.
Squint/Strabismus
A strabismus is any misalignment of the eyes where both eyes do not look in the same direction. Strabismus occurs in 3-4% of the Australian population and may be present intermittently or constantly. Often the misalignment is of just one eye but it may also switch between the two eyes. While children can get a strabismus from as young as 6 months old it more commonly starts to occur in children aged 3-4 years old. Adults may also get a strabismus which often results in double vision.
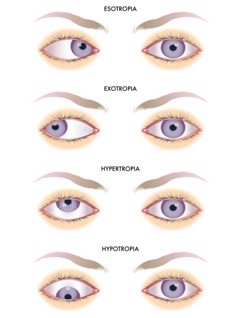
Strabismus is commonly classified by the direction in which the eye turns
- Esotropia – where the eye turns inwards towards the nose
- Exotropia – where the eye turns outwards away from the nose
- Hypertropia – where the eye turns up
- Hypotropia – where the eye turns down
Causes
Nerve Palsies – There are many nerves that supply the 6 muscles on each eye that control our eye movements. If any of these nerves are damaged then they are unable to make the eye muscles they control fully activate. Common causes are damage to the nerves from diabetes, high blood pressure and trauma. The trauma of the birth process can often lead to minor nerve damage, which can in some cases, cause a strabismus.
Eye Muscle Restrictions – Sometimes the muscles around the outside of the eye that control the eye movements become damaged or get trapped. This restricts the eye from moving into a certain position. Often this makes it look like the unaffected eye has gone “too far.” While it can occur in young children this type of strabismus is commonly associated with hyper-thyroidism and injuries to the eye.
Developmental Problems – A child may either have a gross developmental problem that may affect their eyes or a specific problem in the development of the eye, eye muscles or nerves. Well known conditions such as cerebral palsy and Down’s syndrome are commonly associated with strabismus and children diagnosed with these should have an ophthalmic assessment. When the eye muscles or nerves have not normally developed this usually leads to the inability of the child to move their eye into particular directions.
Accommodation – Many children who develop an inward turning strabismus around the age of 4 do so because of their need to focus to see near objects clearly. These children are often longsighted which means to see clearly they need to focus more than a person with normal eyes. This extra focusing causes the eyes to turn in. This type of strabismus can be corrected with appropriate glasses prescribed by the ophthalmologist.
Poor Binocular Control – The brain is the control centre that tries to align our eyes so that we see single, clear vision. Sometimes the effort this requires causes the brain to ‘switch off’ an eye and that eye will drift in or out. Poor binocular control accounts for the majority of intermittent strabismus. Often control can be improved with eye exercises, patching and glasses so that the frequency of the eye turn reduces.
Treatments
Generally if there is any amblyopia associated with a strabismus in a child the amblyopia is treated first. Occasionally this alone will help to realign the eyes. Treatment of the strabismus itself often requires a combination of interventions that may include glasses, eye exercises and eye muscle surgery.
What to do if you suspect your child has a strabismus
Your child will have several very thorough eye examinations the first time they visit South West Vision Institute and often the strabismus becomes readily apparent. However to aid in the consultation it is helpful if you think about which eye is the one that turns and what direction it turns. If you believe your child has a strabismus that isn’t there all the time please bring some photos of your child’s eyes to your consult showing the eye turn.
Strabismus Surgery
Surgery to correct a squint involves operating on the muscles attached to the outside of the eye in order to align the eyes. This is done by either shortening the muscle to make it stronger or by relocating where the muscle is inserted on the eye. Eye muscle surgery cannot correct all strabismus and often there is a high likelihood a second procedure will be required. As with any surgery there are risks of infection and complications however the rates of these are low.
Potential Benefits of Strabismus Surgery
- Improved cosmesis
- Reduced double vision
- Improved binocular control
- Restoration of fine depth perception

Tear Duct Obstruction and Watery Eye
When a baby is born often the tiny ducts that drain the tears out of the eye have not yet fully opened. Frequently the first sign of this is a constantly watery eye where tears run out of the eye and down the baby’s cheek. These children also commonly get repeated episodes of conjunctivitis and are prescribed many courses of antibiotic drops and syrups. It is important during this time to clean the child’s eyes regularly and avoid infecting the other eye. Fortunately 9 out of 10 children with a blocked tear duct will have theirs naturally open by the time they have turned 1 year old.
Treatments
Common treatments for tear duct obstructions include tear duct massage and warm compresses. These encourage the drainage pathway to open. The ophthalmologist may also prescribe antibiotics, where appropriate, to help control any associated conjunctivitis. Surgery is usually a final consideration and aims to manually open the tear duct. As with any surgery there are risks of infection and complications. Currently there has been little research conducted on the long term effects of general anaesthetic and sedation on infants and these effects are stillwidely unknown. Your child’s ophthalmologist will thoroughly explain any surgical considerations with you before you proceed.