Glaucoma
What is Glaucoma?
Glaucoma is known to be one of the leading causes of blindness in the world. Half of Australians affected are unaware or have not been diagnosed.
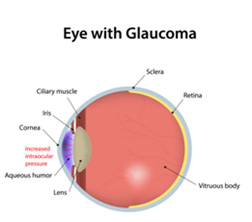
It is an irreversible condition that damages the optic nerve (the nerve connecting the eye to the brain). Poor blood supply to this nerve may also cause glaucoma.
The other cause of this mechanism occurs when there is a build-up of fluid (aqueous humor) from over production or narrowing/blockage of the draining mechanism within the front part of the eye.
Aqueous humor is the fluid produced in the eye that nourishes the cornea (front window of the eye) and lens of the eye. Damage to the optic nerve can eventually cause loss of peripheral vision.
Advance stages of this condition could result in tunnel vision.
What are the risk factors for Glaucoma?
Anyone can be diagnosed with this condition however people will have higher risk of glaucoma if they have the following;
- Family history.
- Diabetes.
- Hypertension.
- Trauma to the eye.
- Migraines.
- Myopia (Short sightedness).
- Hypermetropia (Long sightedness).
- Corticosteroid use in the past or present.
- Smoke cigarettes.
What are the symptoms of Glaucoma?
Certain types of glaucoma can result in high pressure within the eye. This can lead to following:
- Sore painful red eye.
- Blurred vision.
- Haloes around lights.
- Pressure sensation behind the eye.
- Headaches at night.
- Sudden loss of vision.
Advance stage of this disease can result in tunnel vision which can lead to trouble navigating around.
The best way to detect this condition is to see your local optometrist for an eye check-up by the age of 40. It should be sooner from the age of 35 years if you have any of the associated risk factors.
People of the African or the Asian population should have an eye examination by the age of 40 years and the Caucasian population by 50 years of age.
Types of Glaucoma
POAG (Primary Open Angle Glaucoma) – This is the most common and chronic type of glaucoma. It is usually painless and eye pressure above 21 will need to be treated below this.
NAG (Narrow Angle Glaucoma) – People with this type of glaucoma have an anatomically narrow drainage system which means aqueous humor is slower to drain out. This can lead to consistently higher eye pressure. People with is condition are at risk of AACG.
AACG (Acute Angle Closure Glaucoma) – This is an acute condition where the iris (coloured front part of the eye) blocks the drainage system in the front of the eye.
The aqueous humor cannot drain out causing a pressure spike causing blurred vision, painful eye, nausea and vomiting.
NTG (Normal Tension Glaucoma) – The normal pressure in the eye is normally between 10 and 21. However each individual has their own normal.
With this form of glaucoma, patient eye pressure is within the normal range initially and target range will be dependent on a number of factors and the baseline eye pressure.
Secondary Glaucoma – Glaucoma caused by trauma to the eye, cataracts, strokes in the eye, steroid use and inflammatory eye conditions.
Congenital Glaucoma – A child is born with abnormal drainage system or develops it later in life. Child may display excessive watery eyes and light sensitivity as well as appearance of enlarged cloudy eyes
How is Glaucoma diagnosed?
Initially a series of tests and baseline measurements of the eye will need to be performed.
Patient History: Helps determine individual risks.
Corneal Pachymetry: Measures the thickness of the cornea (Front window of the eye).
Applanation Tonometry: Measures the eye pressure.
Gonioscopy: Assesses the drainage network inside the front of the eye for potential narrowing and blockage.
OCT Scans (Optical Coherence Topography): A non-invasive scan of the optic nerve and the nerve fibre bundle layers.
Automated Visual Field Testing:
It is a sensitive test to map the peripheral vision to assess glaucoma damage.


Treatment/Management
Once glaucoma has been diagnosed, patients are usually seen every 6 months to monitor their condition. Usually Applanation tonometry, OCT scan and the automated visual field is performed again.
Eye Drops: Glaucoma is primarily managed by medicated eye drops which are instilled once or several times daily indefinitely. Management of glaucoma may require more than one bottle of medicated eye drop.
SLT (Selective Laser Trabeculoplasty) laser: Used when eye drop therapy is found to be inadequate at lowering eye pressure or causing intolerable side effects.
The laser is fired into the drainage system of the front part of the eye, which stimulates tissue to allow better drainage outflow.
PI (Peripheral Iridotomy) YAG laser: It is used as a preventative treatment when a patient is found to have narrow drainage system and have a higher chance of acute angle closure glaucoma.
It is also used when a patient presents with acute angle closure glaucoma.
Surgery: Surgery is usually performed when eye drops and laser cannot adequately lower the eye pressure. This would involve creating alternative drainage system to allow the aqueous humour to flow out of the eye.
With surgery there is always risk of infection as well as failure to drain the aqueous humor out.